Blood clots are common among senior adults, and present themselves in different ways.
Some of them can cause permanent damage to the body, according to the Centers for Disease Control and Prevention, but many can be treated successfully and decrease the chances of them returning.
Deep Vein Thrombosis (DVT) – Signs and Symptoms
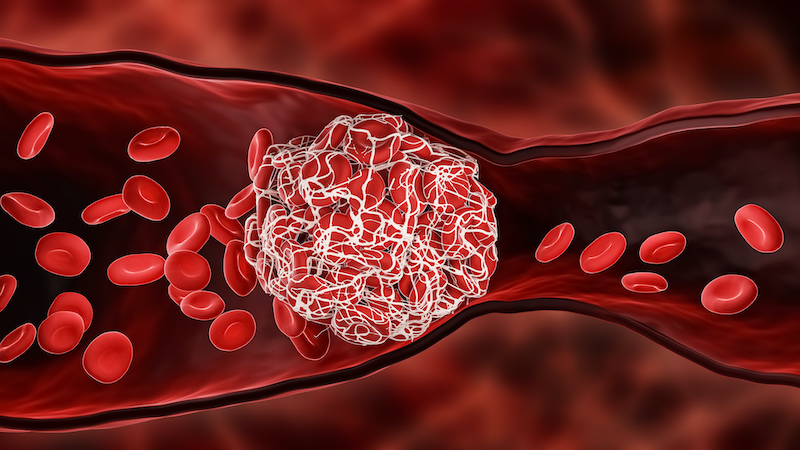
Blood clots are gel-like collections of blood that form in veins or arteries. They are part of the body’s defense to stop the flow of blood due to injury, but if they do not dissolve, they can become dangerous. A clot may stay in one spot or move through a person’s body. It’s the clots that move that are especially concerning.
Deep vein thrombosis (DVT) occurs when a clot forms in one of the body’s larger veins, usually in the legs. If it stays in place, it may not cause harm, but if it dislodges, it can travel to and get stuck in the lungs. This condition is called a pulmonary embolism (PE), and the resulting restriction of the blood flow in the lungs can be fatal. As many as 100,000 people in the U.S. die each year from DVTs and PEs. Even if death does not occur, permanent damage to the lungs and other parts of the body are possible. Because of this, DVTs and PEs are considered medical emergencies that require immediate care.
SYMPTOMS OF BLOOD CLOTS:
- Recent swelling of one leg
- Unexplained pain or tenderness in one leg
- Increased warmth in the area of the leg that’s swollen or painful
- Red or discolored skin on the leg
- Change in color of one leg to blue or purple
SYMPTOMS OF A PULMONARY EMBOLISM:
- Recent or sudden shortness of breath
- Sharp chest pain, especially when breathing in
- Coughing up blood
- Rapid pulse
- Sudden changes in vision
- Sudden weakness or numbness of the face, arm or leg
- Feeling lightheaded or fainting
- Profuse sweating
- Sudden collapse
According to the Cleveland Clinic, blood clots can occur in these areas of the body as well:
Abdomen: Blood clots here can cause pain or nausea and vomiting.
Arms or legs: A blood clot in the leg or arm may feel painful or tender to the touch. Swelling, redness and warmth are other common signs of blood clots here.
Brain: Blood clots in the brain (strokes) can cause a range of symptoms, depending on which part of the brain they affect. These clots may cause problems speaking or seeing, or result in the inability to move or feel one side of your body. Seizures can also occur as a result of brain blood clots.
Heart or lungs: A blood clot in the heart will cause symptoms of a heart attack such as intense chest pain, sweating, pain that travels down the left arm, and/or shortness of breath.
Risk Factors of DVT
Some factors can put seniors at an increased risk for DVT. Those risk factors include:
- Being 60 years old or older
- Injury to a vein due to a fracture, muscle injury and major surgery
- Slow blood flow due to bed confinement, or limited movement
- Long-term sitting or crossing of legs, and prolonged inactivity
- Paralysis
- Chronic diseases such as heart disease, lung disease and Crohn’s disease
- A previous DVT or PE
- A family history of blood clots
- Obesity
- Smoking
- A catheter placed in a central vein
- Clotting disorders (hypercoagulable states) — usually a genetic disorder which increases the tendency to form clots.
How a Pulmonary Embolism is Diagnosed
Diagnosis of a PE can include:
- A blood test
- Chest X-ray
- Ultrasound
- CT scan
- MRI
Treatment
Treatment options can include medications and/or surgery. There are anticoagulant blood clot dissolver medications available by prescription.
Blood thinners can help prevent clots from forming. Regular blood tests may be recommended to monitor how your blood is clotting, especially if a person is taking anticoagulants.
If a clot cannot be dissolved by other means, surgery involving a thin catheter is threaded through the blood vessels to the clot to remove it.
Preventing Blood Clots
There are ways to lessen the chances of developing a blood clot, such as:
- Regular exercise
- Maintaining a healthy body weight
- Staying hydrated
- Abstaining from smoking
- Moving regularly—standing and walking periodically, moving your legs and feet
- Avoiding placing pillows under the knees and sitting in positions where knees and hips are sharply bent
- When sitting, elevating your feet to prevent blood from pooling
- Wearing compression stockings (consult with your physician first)
If you suspect DVT or PE, contact your physician or proceed to a hospital immediately.
The Latest on Taking Aspirin
For many years, people were advised to take low-dose aspirin as a blood thinner.
Recently the guidelines have changed regarding low-dose aspirin.
Some people who are at an increased risk for a heart attack or stroke may still benefit from this regimen. Others who are not at risk for heart disease, stroke, or have not received stents or undergone heart surgery and do not have significant atherosclerosis (clogging of the arteries) may not benefit from low-dose aspirin.
While aspirin does interfere with the forming of blood clots, it also increases the risk of bleeding.
The bottom line: All seniors should consult with their physician about taking or not taking low-dose aspirin.
Check out Bethesda’s Health & Wellness blog for more preventive care tips.
Want to find out more?
If you’d like to stay up to date with Bethesda Health Group, sign up here to receive our blog and newsletters!
"*" indicates required fields
Related Articles
Want to find out more?
If you’d like to stay up to date with Bethesda Health Group, sign up here to receive our blog and newsletters!
"*" indicates required fields